Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-qformat:yes;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin-top:0in;
mso-para-margin-right:0in;
mso-para-margin-bottom:10.0pt;
mso-para-margin-left:0in;
line-height:115%;
mso-pagination:widow-orphan;
font-size:11.0pt;
font-family:”Calibri”,”sans-serif”;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;
mso-bidi-font-family:”Times New Roman”;
mso-bidi-theme-font:minor-bidi;}
Diabetic sores, a common complication among individuals with diabetes, present challenges that require careful attention, proactive management, and specialized care to promote healing and prevent complications. These sores, often stemming from neuropathy or poor circulation, demand a comprehensive approach tailored to individual needs.
Key aspects integral to managing diabetic sores include:
- Early Detection and Assessment: Prompt identification and continual monitoring of sores, paying attention to their location, size, and any signs of infection, are crucial. Regular foot examinations are essential to catch issues early.
- Optimal Wound Care: Proper wound care involves cleansing the sores with mild solutions, applying appropriate dressings, and keeping the area clean and protected. Debridement may be necessary to remove dead tissue and promote healing.
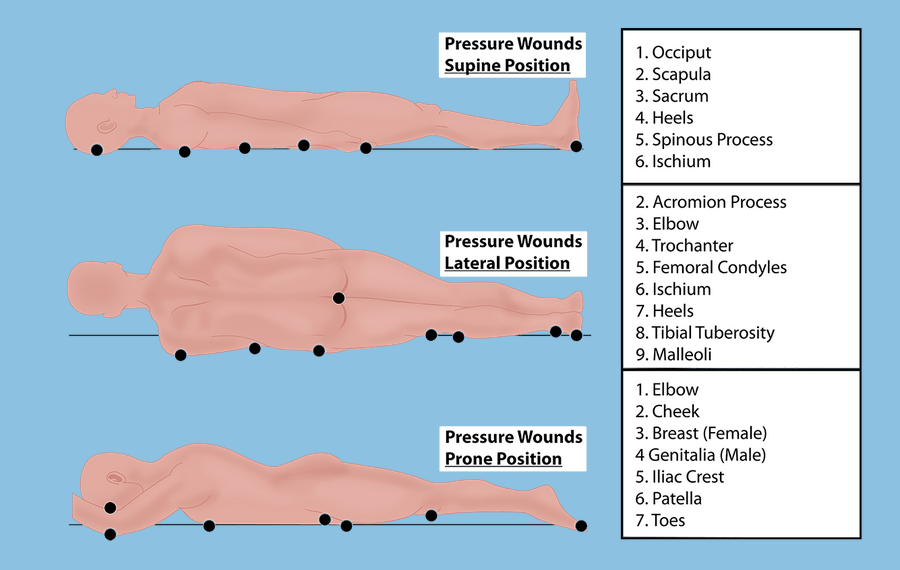
- Offloading Pressure: Reducing pressure on affected areas is vital for healing. Special footwear, padding, or orthotic devices can help redistribute pressure and alleviate stress on the sores.
- Comprehensive Diabetes Management: Managing blood sugar levels through medication, diet, and lifestyle adjustments is pivotal. Controlled glucose levels aid in preventing further complications and support the healing process.
Collaboration among a multidisciplinary healthcare team, including podiatrists, wound care specialists, endocrinologists, and nurses, is essential. Their combined expertise ensures a holistic approach to managing diabetic sores, addressing both the wound and underlying factors.
Diabetic sores not only affect physical health but can also impact emotional well-being and mobility. Patient education on foot care practices, preventive measures, and early warning signs empowers individuals to actively participate in their healing and prevent future issues.
Investments in research and innovative therapies demonstrate a commitment to improving diabetic sore management. Ongoing advancements aim to enhance healing rates, reduce complications, and enhance the quality of life for those affected by diabetes-related wounds.
Managing diabetic sores involves a proactive, informed, and compassionate approach. It’s about fostering healing, preserving mobility, and supporting individuals in navigating the challenges associated with diabetes-related complications.